Journal: The Journal of Vascular Access
Author: Emanuele Gilardi
Publication Date: 2022
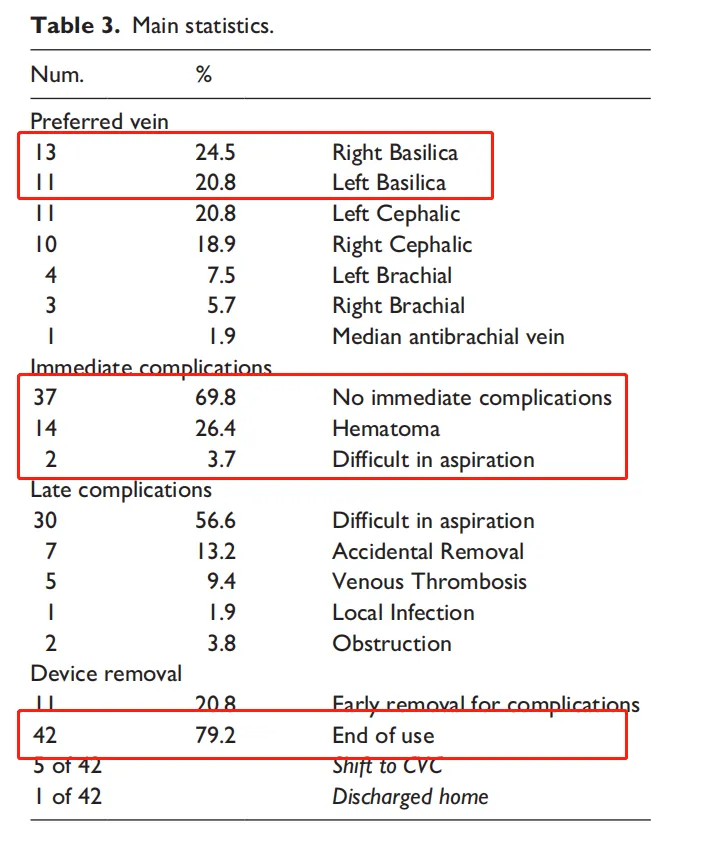
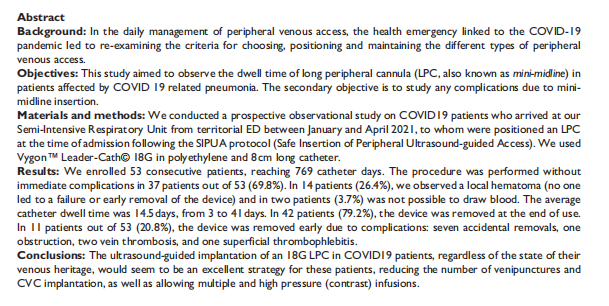
Objective: This study aims to observe the dwell time of mini midline catheters in COVID-19 patients, with a secondary objective of investigating complications related to the insertion of mini midline catheters.
Methods: A prospective observational study was conducted on COVID-19 patients admitted to a semi-intensive respiratory ward from the regional emergency department between January and April 2021. Upon admission, patients received an 18G 8cm mini midline catheter inserted according to the SIPUA protocol (Safe Insertion of Peripheral Ultrasound-guided Access).
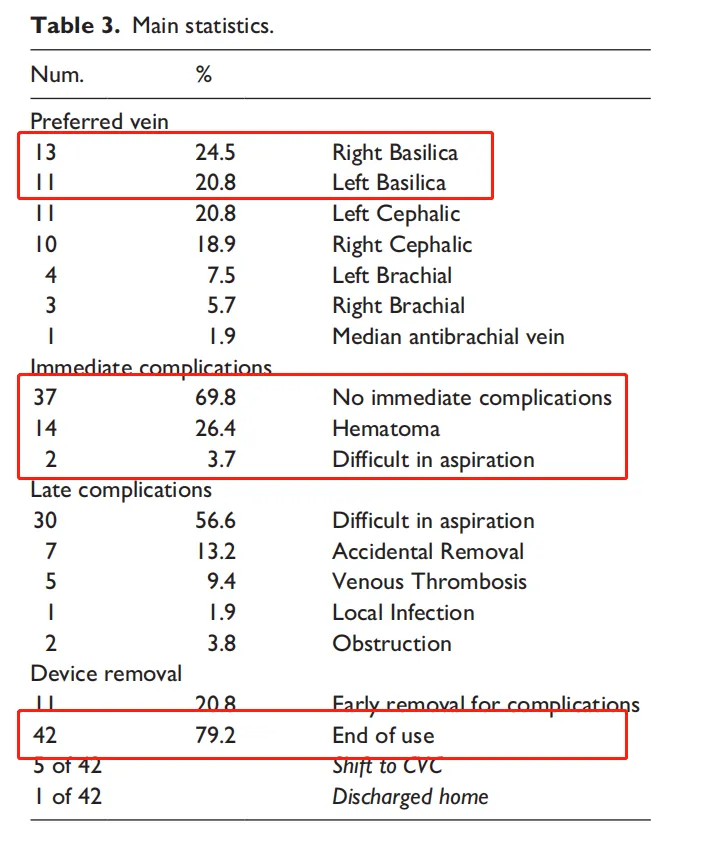
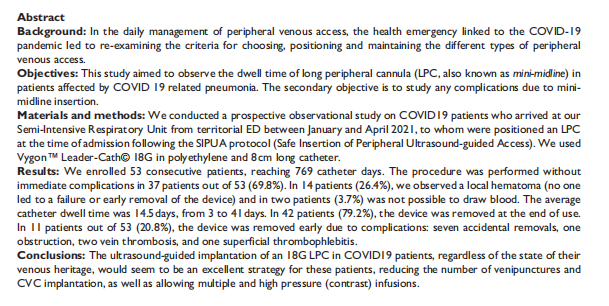
Results: A total of 53 patients were consecutively enrolled, accounting for 769 catheter days. Among the 53 patients, 37 (69.8%) underwent the procedure without immediate complications. Local hematomas were observed in 14 patients (26.4%), which did not lead to catheter dysfunction or premature removal. Difficulty in blood aspiration was noted in 2 patients (3.7%). The average catheter dwell time was 14.5 days.
Conclusion: The insertion of mini midline catheters under ultrasound guidance is an excellent strategy for COVID-19 patients, regardless of their venous condition. It reduces the number of venipunctures and central venous catheter (CVC) insertions, and allows for multiple high-pressure (contrast agent) infusions.
Background:
1. The COVID-19 pandemic has led to significant changes in clinical practice, particularly in the daily management of peripheral venous access. Based on the latest therapeutic evidence, it is necessary to reselect and reposition infusion tools for the appropriate treatment of COVID-19 patients.
2. COVID-19 patients can induce a hypercoagulable state, necessitating a safe and stable venous access.
3. Mini midline catheters, inserted using the SIPUA protocol (Safe Insertion of Peripheral Ultrasound-guided Access), have proven effective in reducing the number of venipunctures, increasing satisfaction among patients and healthcare professionals.
Study Subjects and Methods:
A prospective observational study was conducted on COVID-19 patients with the following inclusion criteria:
1. Admission diagnosis of "acute respiratory failure due to interstitial pneumonia caused by SARS-CoV-2 infection."
2. Patients over 18 years of age who provided informed consent for the study.
.png)
Environmental and Procedural Preparations:
1. Hand hygiene, aseptic technique, and protective equipment
2. Preoperative ultrasound assessment
3. Selection of the most suitable vein
4. Ultrasound evaluation of nerves and brachial artery before venipuncture
5. Ultrasound-guided puncture
6. Aspiration of blood and flushing with saline
7. Securing the catheter with a device
8. Documentation
Study Results:
.png)
Among the 53 patients:
• Average age: 71.1 years
• Average procedural time: 12.1 minutes
• Average dwell time: 14.5 days
• Average vein diameter: 4.5 mm
• Average vessel depth: 10.4 mm
• 24 patients (45.2%): Preferred basilic vein
• 37 patients (69.8%): Underwent the procedure without immediate complications
• 14 patients (26.4%): Local hematoma (did not lead to catheter dysfunction or premature removal)
• 2 patients (3.7%): Difficulty in blood aspiration
• Average catheter dwell time: 14.5 days, with 42 patients (79.2%) having the catheter removed after treatment, and the longest use being 41 days.
Conclusion:
The insertion of mini midline catheters under ultrasound guidance for hospitalized patients with SARS-CoV-2 pneumonia is an excellent strategy regardless of their venous condition. Mini midline catheters are highly versatile in all emergency situations, ensuring stable and safe venous access. Compared to peripheral intravenous catheters, they reduce the number of venipunctures, save resources, and decrease healthcare workers' exposure to infection, sometimes even avoiding the need for central venous catheter (CVC) insertion.






.png)
.png)