【Literature Interpretation】Safety and efficacy of vasopressor administration through midline catheters
Original Text:Safety and efficacy of vasopressor administration through midline catheters
Journal: Journal of Critical Care
Confirming the safety and effectiveness of vasoactive medication infusion via midline catheter is the main goal of this investigation.
Methods: A retrospective analysis of the clinical application of a midline catheter in a 600-bed tertiary teaching hospital's intensive care unit between 2016 and 2019.
Results: No inefficient administration or problems linked to the limbs occurred during the infusion of vasoactive medications via a midline catheter in 248 patients.
Conclusion: Vasoactive medications can be administered for extended periods of time safely and effectively with midline catheters, which are a safe substitute for CVCs.
Background
Vasoactive agents are frequently used as a treatment for critically ill patients who are hemodynamically unstable. These agents are infused through a central venous catheter (CVC), putting patients at risk for thromboembolic, mechanical, and infection-related complications. In fact, catheter-associated bloodstream infections from vasoactive drug infusions account for one-third of the mortality factors linked to hospital-acquired disease (HAC).Eighty-five percent of issues happen farther away from the upper extremity's anterior elbow fossa. The most common complication is an indwelling needle infusion in a small vein in the hand or foot, which significantly increases the risk of exudate.- A midline catheter (MC) that ends in a longer catheter in a larger vein has a significantly lower incidence of phlebitis than an indwelling needle. A longer indwelling time (2-4 weeks), a longer infusion possible, and a lower risk of weaning and exudation- Earlier removal of the central venous catheter or replacement by peripheral intravenous infusion access is more preferred in clinical practice. The rate of catheter-associated bloodstream infections with midline catheters is 0% to 0.9%, which is close to that of an indwelling needle
Method
Methods: Retrospective study
Research period: 2016-2019
Study site: Intensive care unit at George Washington University Hospital (including medical, surgical, trauma, and neurosurgical patients
Subjects: Patients aged ≥ 18 years who were admitted to the ICU for infusion of vasoactive drugs (phenylephrine, norepinephrine, epinephrine, angiotensin II, etc.) through a midline catheter
Data collection: Midline catheter placement indications duration of use complications, peripheral vascular active drug treatment duration, drug type, drug concentration and other data were recorded
Statistical analysis: Analysis using SAS version 9.4
Result
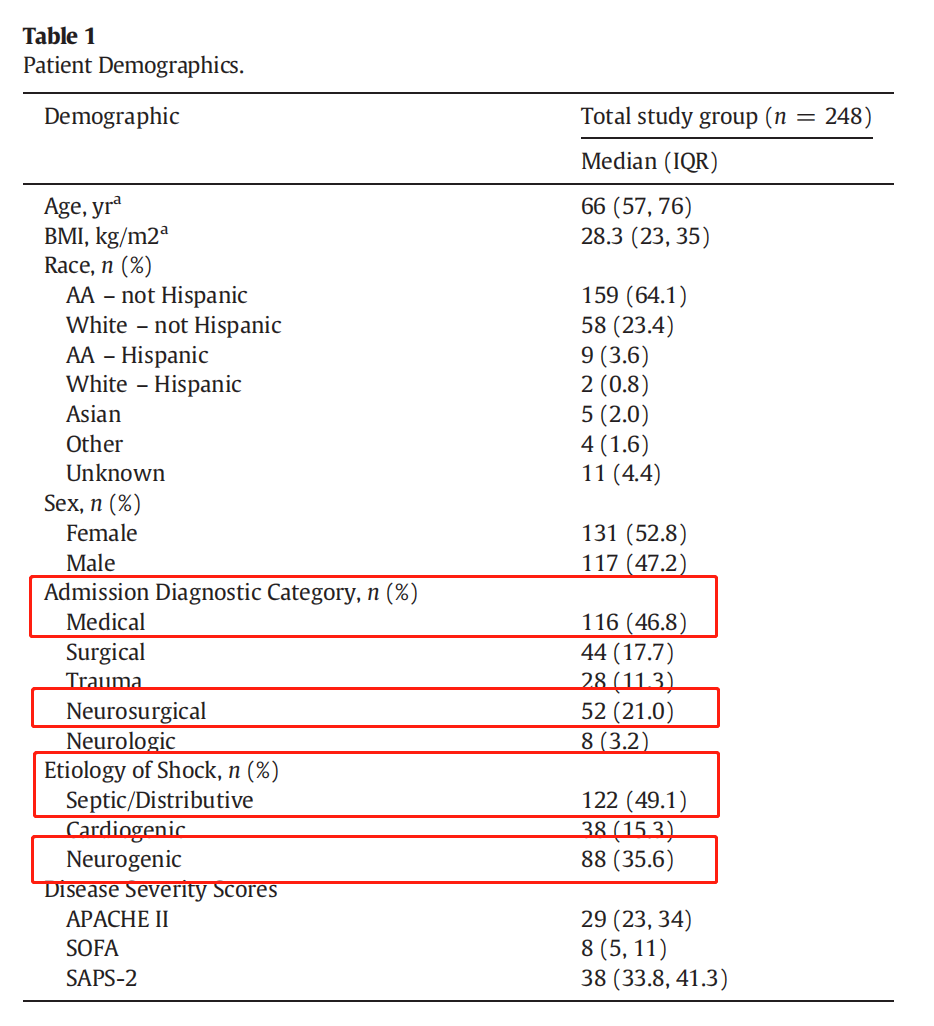
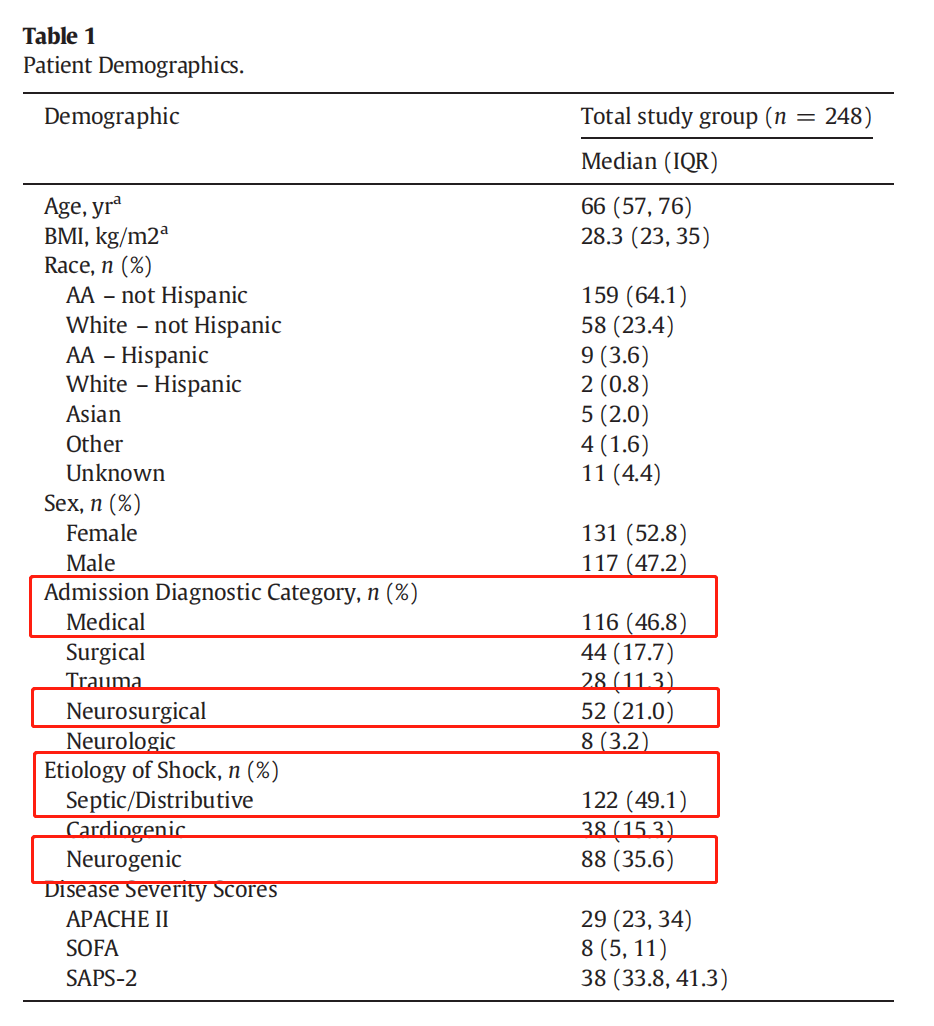
- A total of 248 patients were injected with vasoactive drugs through midline catheter within the specified time period.
- Population statistics: Patients in medical intensive care (46.8%)
- Patients after neurosurgery (21%)
- Infectious or distributed shock secondary circulatory shock (49.1%)
- Neurogenic diseases such as spinal cord injury after craniotomy (35.6%)
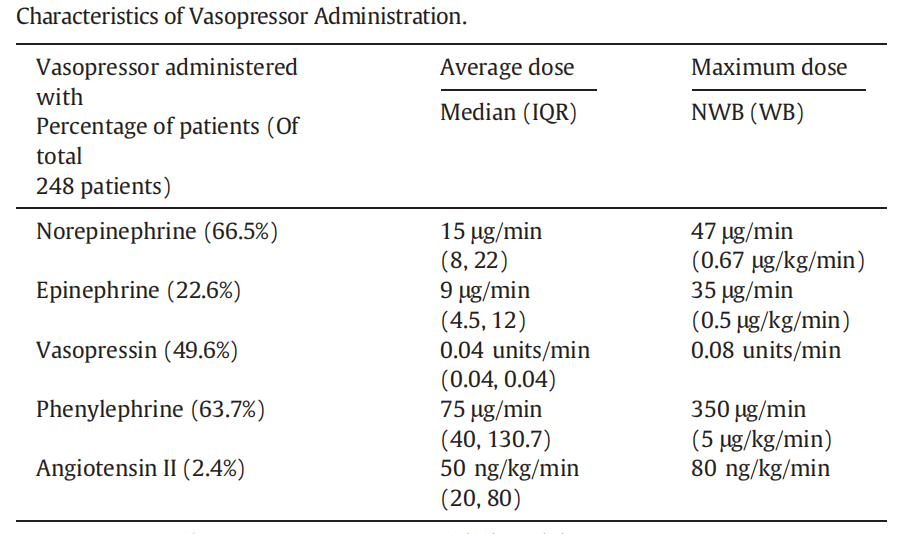
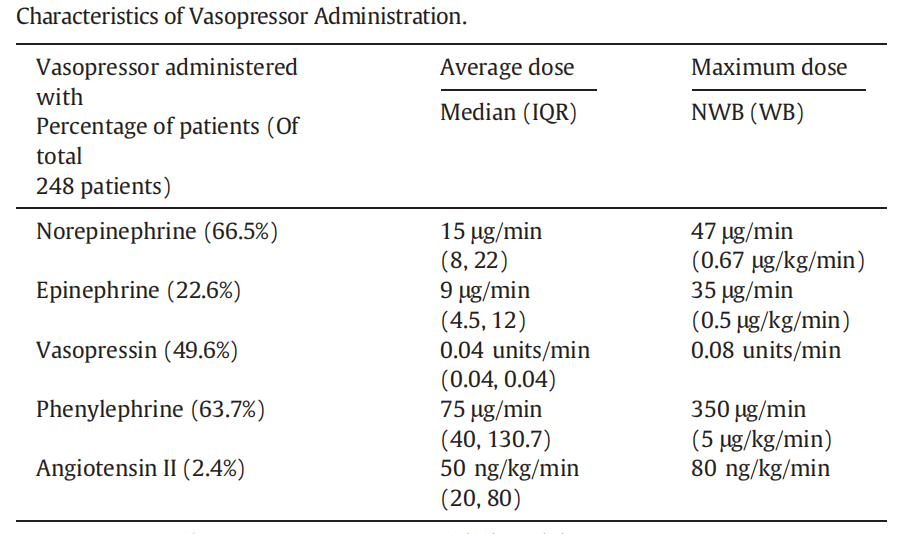
2) Drug statistics:
Common infusion drugs: norepinephrine 66.5%, phenylephrine 63.7%
Average continuous infusion time of vasoactive drugs: 7.8±9.3 days
Drug concentration:
Norepinephrine: 8mg/250mL normal saline
Epinephrine: 8mg/250mL 5% glucose
Vasopressin: 40U/100mL 5% glucose
Phenylephrine: 10mg/250mL 5% glucose
Angiotensin II: 2.5mg/250mL normal saline
3)Catheterization statistics:
Success rate of one-time catheterization: 97.6% (n=242)
Vascular selection: 98.8% (n=245)
Average indwelling time: 14.7±12.8 days
Complications: 3.2% (6 cases of unknown infection, 1 case of exudation, 1 case of phlebitis), no ineffective administration or limb-related complications, all patients were discharged under extubation.
Conclusion
The midline catheter can be used as a bridge between the peripheral indentation needle and CVC, particularly in patients with veins that are difficult to puncture. Its benefits include a long retention period, low infection rate, fewer repeat punctures, and increased patient satisfaction. For patients who require prolonged vasoactive medication, the midline catheter can be utilized as an early option to shorten the duration of CVC indentation and prevent CLABSI.
Revelation
- The midline catheter effectively completes the treatment plan of vasoactive drug.
- infusion in critically ill patients and eliminates the need for an X-ray for continuous and relatively long (7.8±9.3 days) vasoactive infusions; it also solves the catheterization problem in patients with obesity, edema, circulatory failure, or nearly no remaining superficial veins after repeated venipuncture.
c.The implantation of the midline catheter can save a large deal of money on medical expenses by reducing the number of CVC days and the rate of CLABSI.