Journal: Journal of Clinical Medicine
Publication Date: 2024
Objective: To compare the short-term prognosis of tunneled central catheters (TCC) and non-tunneled central catheters (NCC) in acute hemodialysis patients, with a particular focus on infection rates, dislocation rates, and thrombosis rates within the first three weeks post-insertion.
Methods: A retrospective analysis was conducted on 176 hemodialysis catheters placed between January and December 2023 at Policlinico di Modena and Ospedale Civile di Baggiovara. Patient demographics and complications were recorded at the time of catheter insertion. The outcomes assessed included catheter-related infections, dislocation rates, and thrombosis.
Results: Of the 176 catheters, 127 were TCCs and 49 were NCCs. The infection rates for TCC and NCC were 3.15% and 8.16%, respectively. The dislocation rates were 0.79% for TCC and 4.08% for NCC. There was one case of thrombosis in the NCC group.
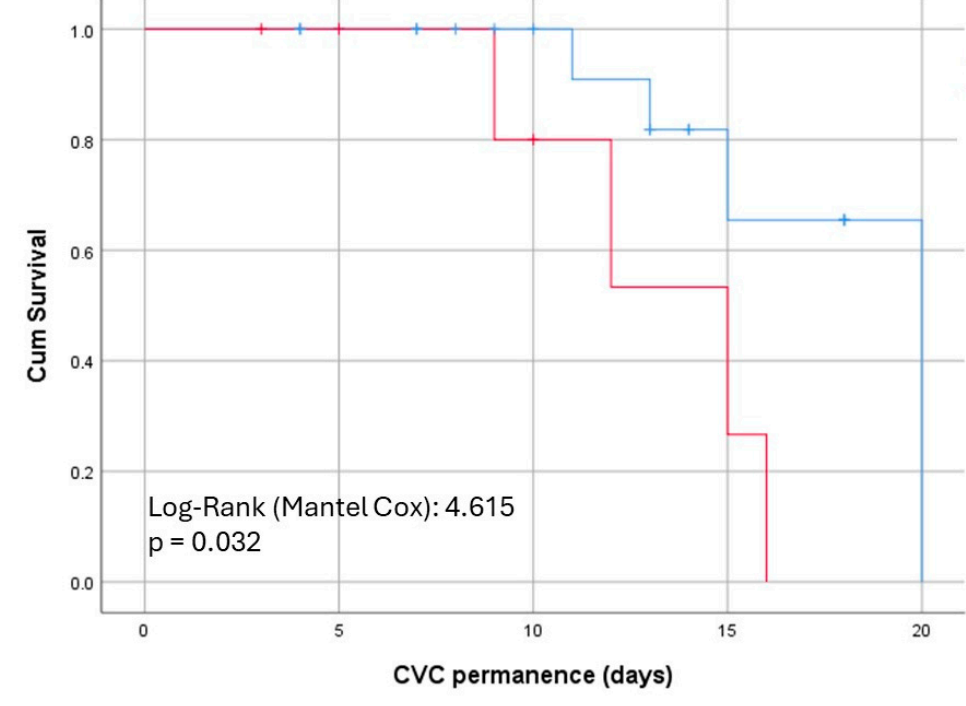
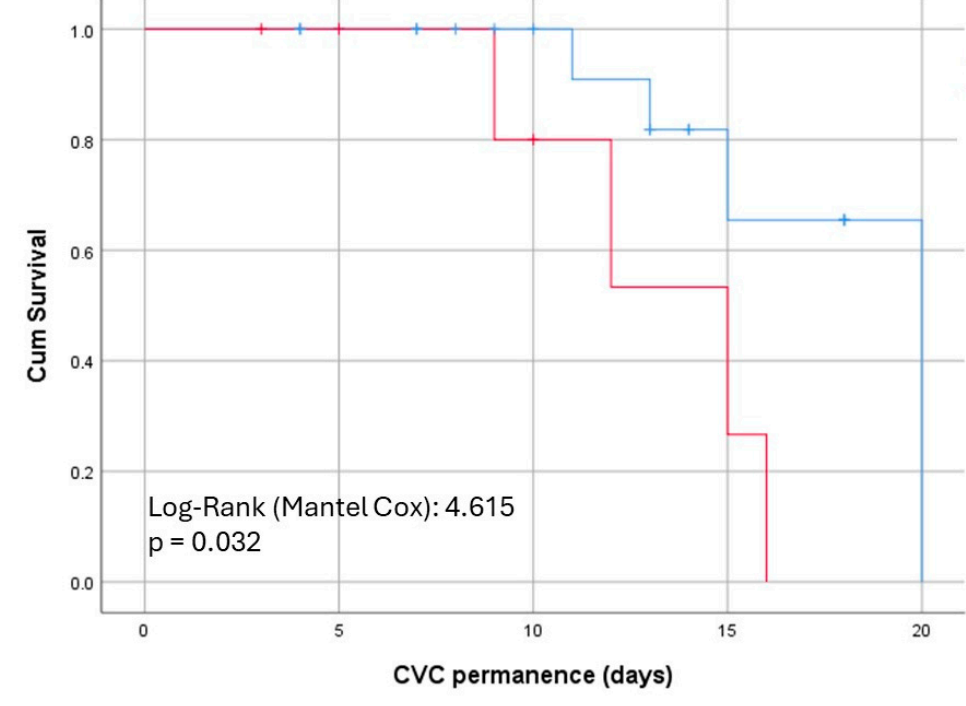
Conclusion: Compared to TCC, NCC does not significantly alter short-term prognosis, but TCC shows better infection-related survival after 10 days. Therefore, initial insertion of TCC may be preferable when resources and clinical conditions allow.
Background:
Despite widespread efforts to increase the use of arteriovenous fistulas globally, the use of hemodialysis catheters continues to rise. From 1996 to 2007, the use of catheters among hemodialysis patients in many countries increased by 1.5 to 3 times. A significant proportion of newly diagnosed end-stage renal disease (ESRD) patients (58%-73%) rely on catheters to initiate hemodialysis. The continued use of hemodialysis catheters highlights their indispensable role in contemporary nephrology.
Hemodialysis catheters are mainly divided into tunneled cuffed catheters (TCC) and non-tunneled catheters (NCC). Traditionally, TCCs are designed for long-term use to reduce infection risk, while NCCs, due to their higher complication rates, are intended for short-term access. The KDIGO guidelines recommend replacing or removing NCCs within two weeks. However, some centers continue to use NCCs for months to years to meet management needs or in resource-limited settings.
Matthew J. Oliver's review observed that the infection risk between the two types of catheters may not be as clear-cut as previously thought. Studies have found that the infection rate of TCCs is higher than that of NCCs, possibly due to the shorter usage time of NCCs. In fact, the risk of bacteremia is closely related to the prolonged use of NCCs.
The choice between TCC and NCC remains a highly debated topic. Previous studies have found differences in infection rates, mechanical complications, and patient survival between these catheter types. Understanding these factors is crucial for optimizing hemodialysis treatment and improving patient outcomes.
Objective:
This study aims to evaluate whether the immediate insertion of TCCs is more advantageous than the initial use of NCCs in acute patients. By comparing the short-term outcomes of these two catheter types, the primary endpoints include catheter-related infection rates, dislocation rates, and thrombosis rates.
Methods:
Study Design: Retrospective study
Study Period: January 1, 2023, to December 31, 2023
Study Location: Policlinico di Modena and Ospedale Civile di Baggiovara
Study Population: All patients who received TCC or NCC for hemodialysis at the two hospitals during the specified period
Insertion Technique: Ultrasound-guided insertion
Data Collection: Demographic information (age, gender, underlying diseases), type of catheter inserted (TCC or NCC), and specific outcomes within the first three weeks post-insertion (catheter-related infections, dislocation, and thrombosis)
Results:
A total of 176 catheters were inserted, with data collected for the first three weeks post-insertion:
Catheter Types: 127 TCCs, 49 NCCs
Adverse Events: 7 in the TCC group, 19 in the NCC group
Catheter-Related Bloodstream Infections: 3.12% for TCC, 8.16% for NCC
Dislocation Rates: 0.79% for TCC, 2.04% for NCC
Thrombosis Rates: None for TCC, 2.04% for NCC
Kaplan–Meier curve analysis comparing the time to catheter removal due to infection events between TCC (blue line) and NCC (red line) showed a significant difference starting around day 10.
Conclusions:
The results of this study suggest that primary insertion of TCCs may be the preferred method for acute hemodialysis patients when resources and operator expertise allow. Compared to NCCs, TCCs have a lower infection risk after the initial 10 days, supporting their use for better long-term outcomes.
Implications:
After 10 days of catheter use, TCCs show a lower infection rate compared to NCCs, supporting the superior infection-related survival of TCCs. This finding aligns with the KDIGO guidelines, which recommend replacing NCCs within two weeks to reduce infection risk.
Acute patients typically recover function around two weeks, so many will require a second catheter replacement from NCC to TCC, even if dialysis is soon discontinued. The necessity of catheter replacement underscores the importance of initial catheter choice and the potential benefits of selecting TCCs when clinically feasible.
Initial insertion of TCCs may present challenges, such as the patient's clinical condition and the operator's expertise. In such cases, using NCCs is reasonable and does not result in higher short-term complication rates. However, in the absence of these barriers, it is preferable to use TCCs immediately. This approach aligns with infection prevention strategies and reduces the need for subsequent catheter replacements, minimizing additional interventions and associated risks.
The economic and follow-up implications of multiple catheter insertions should be considered. Each additional catheter insertion carries risks of complications, increased medical costs, and patient discomfort. By choosing TCCs initially when appropriate, patient outcomes can be improved, and the overall burden on healthcare resources may be reduced.